Disempowering, not insightful

"You don't need to have too much self-control" is the key issue.
Because GLP-1 meds are a ‘brute force’ approach that ‘override the system’ of satiety and food choices, they cover up problems instead of addressing them, a bit like “patching a wall when the foundation is rotting”.
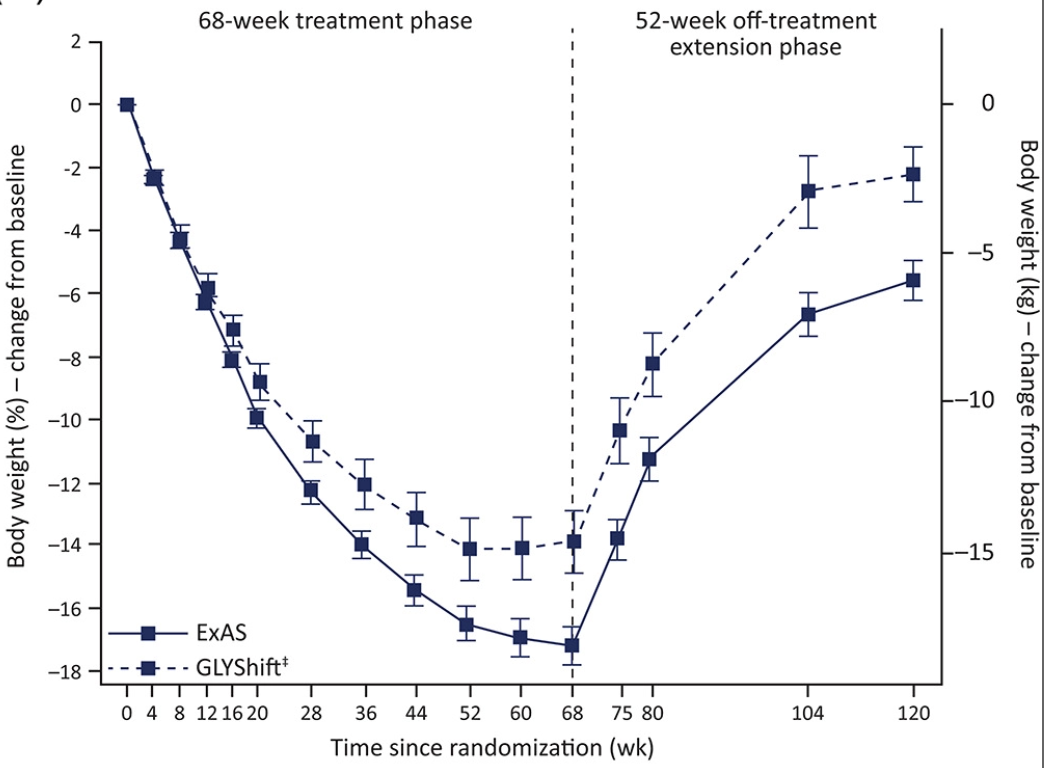
This is not only short-termist and very expensive, it’s also disempowering. The fundamental Big Pharma message is “don’t worry about the causes of obesity, and your role in it — just pay your money, take the meds, and trust us.” There’s no education about food and the body, no illumination of what causes obesity or weight loss, no enhanced understanding. And weight loss without understanding always leads to regain, as nothing has changed in the person’s behaviour around food. Same behaviours, same end result.
Beyond even that, some people (and this is anecdotal) report gaining back more weight than they lost. It’s early to say, but one possible explanation: building up months of desire to eat enjoyable foods, and suddenly finding (after stopping injections) that they are no longer nauseating.
To understand the importance of a feedback loop and behavioural change, see the Limbo loop.
Side effects
The other notable downsides are side effects, including nausea, vomiting, diarrhoea and constipation, with some reporting feeling weak or tired, dizziness, and insomnia. Injection site reactions such as bruising, pain or a rash are occasionally reported. Some people, including Musk, report “rotten egg burps.” On a personal level, many people are averse to needles, so self-injecting can be a challenge.
Long-term questions and concerns
Finally, and very important, the long term effects are still in question, as these are relatively new drugs. As Dr Gareth Nye at Chester Medical School says, “The response to blood sugar is one aspect of hundreds that work together like an orchestra in the body. Taking Ozempic disrupts not only one feedback loop, but hundreds.”
It can facilitate changes in intestinal health, impact the body’s ability to absorb nutrients, and cause inflammation in the pancreas or gall stones. It also affects the subtle interplay of nerves — vagal activities, dopamine response — and the body’s ability to regulate satiation. Finally, there are some major “unknown unknowns” as we have no long term studies on pleiotrophic effects down the gut, and many other potential issues that may appear later — when millions of people have already been injected.
Conclusion
With the media attention and a spate of celebrity endorsements (Kevin Kline! Queen Latifah!), we’re seeing a major assault by pharma companies to medicalise obesity as a ‘chronic disease’ that can only be addressed by medication in perpetuity. But there are serious downsides to consider, especially the high risk of the “yo-yo effect” reverting to prior body weight after stopping the injections.
Article footnotes
^ The Lancet (https://www.thelancet.com/journals/lancet/article/PIIS0140-6736(18)31773-2/fulltext)
^^ The Journal of Pediatrics (https://www.jpeds.com/article/S0022-3476(21)00432-7/fulltext)
^^^ https://www.fda.gov/drugs/postmarket-drug-safety-information-patients-and-providers/liraglutide-marketed-victoza-information
^^^^ https://www.mayfairweightlossclinic.co.uk/treatment/ozempic/
^^^^^ https://jamanetwork.com/journals/jama/fullarticle/2777886